Can cannabis help with Post-Traumatic Stress Disorder?
With wars still raging around the world, many people live in fear and uncertainty. These experiences can lead to Post-Traumatic Stress Disorder (PTSD). While therapy and medication can help, they don’t work for everyone. That’s why more people are exploring alternatives—like cannabis. Once mainly known as a recreational drug, cannabis is now being taken more seriously as a possible treatment. In this article, we explore whether cannabis could help people with PTSD and what science has to say about it.
What is PTSD and how is it treated?
PTSD can develop after experiencing or witnessing a traumatic event. It is characterized by flashbacks, nightmares, trouble sleeping, hyperarousal and avoidance of places, people, or situations reminding of the trauma1. Around 3.9% of the global population will experience PTSD at some point in their lives2. However, the rates are much higher among those exposed to violent conflict or war (15.3%)2. PTSD is typically treated with a combination of psychotherapy and prescription medication. Unfortunately 40-50% of individuals don’t respond to current treatments3.
Can cannabis be a treatment option for PTSD?
In recent years, cannabis-based medicinal products have gained attention as a potential new treatment for PTSD. The focus is on the body’s endocannabinoid system (ECS), which plays a role in regulating stress, emotional memory, and the processing of fear—all important factors in PTSD. Compounds in cannabis, particularly THC (tetrahydrocannabinol) and CBD (cannabidiol), interact with this system, which has led researchers to wonder whether these substances might ease PTSD symptoms4.
What does research say about cannabis & PTSD?
So far, research on cannabis for PTSD is still limited. A recent meta-analysis, which included only ten studies, showed mixed results: about half of the studies reported therapeutic benefits, while the other half found no effect or even a worsening of symptoms5. The most promising results were seen in improved sleep and fewer nightmares.
What about real-world data?
There is growing interest in using Real-World Data (RWD)—information gathered from actual clinical practice, such as electronic health records or patient surveys6. One recent study followed 269 people diagnosed with PTSD for up to 18 months7. Participants reported improvements in PTSD symptoms, anxiety, sleep, and quality of life. However, it is important to note that 74% of the participants were already using cannabis when the study began, which may have influenced the results.
So what can we conclude about cannabis & PTSD?
At this time, there is no strong scientific evidence supporting cannabis as a reliable treatment for PTSD. Most studies so far have focused on male military personnel and veterans, making it also unclear whether the findings apply to women or people who have experienced other types of trauma. Additionally, many of the studies are observational, meaning they cannot show whether cannabis is more effective than a placebo or standard treatments. More high-quality research—including well-designed clinical trials and real-world data—are needed to determine whether cannabis is a safe and effective long-term treatment option for PTSD.
Cannabinoids – Cautions and risks
The cannabinoids THC and CBD 8, 9 are not benign drug substances. THC is psychoactive, euphorigenic, and may have intoxicating effects. 10 The regular, heavy and abusive use of high doses of THC may increase the risks of symptoms of poor mental health, is associated to polydrug use, drug harms, and poor social outcomes. 11 CBD is psychoactive, is not intoxicating, and has physiological side effects; however, little is known about the long-term use of high doses of CBD.
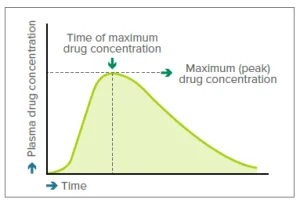
Patients
Most patients tolerate cannabis and cannabis-based medicines well. Side effects are generally dosedependent. However, there are a number of known medicine interactions, contraindications, and side effects. Absolute contradictions include psychosis, and severe depression and anxiety. Some patients may currently use cannabis recreationally or have a history of such use. While there is a lower risk of misuse in a therapeutic context, some patients may self-escalate their dose beyond what was prescribed. Risk factors for problematic cannabis use include prescribing high doses of THC, previous problematic substance use (controlled drugs or alcohol or tobacco), males aged 18-30 years, misuse of controlled drugs at an early age, and current or previous episode of major depression.
Risk of psychosis
In general, patients with a hereditary risk of psychosis or other psychiatric conditions (schizophrenia or major depressive disorders) should avoid the use of THC containing medicines, as they may worsen the condition. Drug induced anxiety and depression is possible in the case of non-predisposed individuals, especially when high doses of THC are used.
A clinical primer
a guide to the rational use of cannabis-based medicines
The therapeutic effects of cannabis are mainly attributed to Δ-9-THC (delta-9-tetrahydrocannabinol) and CBD (cannabidiol). The evidence base for prescribing medicinal cannabis is well defined. So far only a few health conditions are supported with published clinical research and knowledge of good clinical practice.
The booklet ‘A clinical primer – a guide to the rational use of cannabis-based medicines’ is a clinical guidance text and should be referred to by prescribers, pharmacists and nurses.
The Appendix: Clinical evaluation tools, provides clinical screening and evaluation tools used to assess the patients risk of cannabis misuse, and for screening for anxiety and depression before prescribing medicines containing THC.
References
- American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.)
- Koenen KC, Ratanatharathorn A, Ng L, McLaughlin KA, Bromet EJ, Stein DJ, et al. Posttraumatic stress disorder in the World Mental Health Surveys. Psychol Med. 2017 Oct;47(13):2260–74. doi:10.1017/S0033291717000708.
- Green B. Post-traumatic stress disorder: new directions in pharmacotherapy. Adv Psychiatr Treat. 2013;19(3):181–190. doi: 10.1192/apt.bp.111.010041
- Hill, M., Campolongo, P., Yehuda, R. et al. Integrating Endocannabinoid Signaling and Cannabinoids into the Biology and Treatment of Posttraumatic Stress Disorder. Neuropsychopharmacol. 43, 80–102 (2018). https://doi.org/10.1038/npp.2017.162
- Rodas, J. D., George, T. P., & Hassan, A. N. (2024). A systematic review of the clinical effects of cannabis and cannabinoids in posttraumatic stress disorder symptoms and symptom clusters. The Journal of clinical psychiatry, 85(1), 51827.
- Real-World Evidence—What Is It and What Can It Tell Us? The New England Journal of Medicine, Dec. 6, 2016
- Datta, A., Erridge, S., Warner-Levy, J., Clarke, E., McLachlan, K., Coomber, R., … Sodergren, M. H. (2025). UK medical cannabis registry: an updated clinical outcomes analysis of patients with post-traumatic stress disorder. Expert Review of Neurotherapeutics, 25(5), 599–607. https://doi.org/10.1080/14737175.2025.2490539
- ∆-9-THC (THC): delta-9-tetrahydrocannabinol; CBD: cannabidiol.
- Other relevant, topical, cannabinoids include ∆-8-THC which is derived from CBD through chemical industrial process.
- WHO. ICD-10. Intoxication is a transient condition that follows the administration of a psychoactive substance and results in disturbances in the level of consciousness, cognition, perception, judgement, or behaviour, or other psycho-physiological functions and responses.
- Lynskey, M. and W. Hall, The effects of adolescent cannabis use on educational attainment: a review. Addiction, 2000. 95: p. 1621-1630.
Fergusson, D. and J. Boden, Cannabis use and later life outcomes. Addiction, 2008. 103: p. 969-976.
Iversen, L., Cannabis and the brain. Brain, 2003. 126: p. 1252-1270.
Di Forti, M., et al., High-potency cannabis and the risk of psychosis. British Journal of Psychiatry, 2009. 195(6): p. 488 – 491.
Frisher, M., et al., Assessing the impact of cannabis use on trends in diagnosed schizophrenia in the United Kingdom from 1996 to 2005. Schizophrenia Research, 2009. 113(2-3): p. 123128.
Fergusson, D., et al., Cannabis and psychosis. BMJ, 2006. 332: p. 172 – 175.
Burggren, A., et al., Cannabis effects on brain structure, function, and cognition: considerations for medical uses of cannabis and its derivatives. Am J Drug Alcohol Abuse., 2019. 45(6): p. 563–579.